(Trigger warning: This blog post describes and shows images of infant surgery, pre and post operation; reader discretion is advised)
When my daughter, Avery finally went into the wait list for gastrostomy surgery, I scoured the internet for any kind of indication of what it would be like, how long would the surgery last? Would she be in pain? What would the stoma look like?
The unknown can be scary in any situation. I had so many questions, and now that my daughter is home and recovered from her g tube surgery, I wanted to create this blog post for those parents that are searching for those same questions that I wanted the answers to.
My daughter was referred for her gastrostomy in June 2021, she had the NG tube for over a year, so I had plenty of time to do my research and discuss our options with Avery’s medical professionals, the g tube was the right option for us.
If you’d like to hear my opinions on the G tube vs NG tube you can check out my blog post where I cover a lot of the good and bad in both.
https://mummyandavery.com/ng-tube-or-g-tube
Meeting The Surgeon
It took 7 months to finally get an appointment with the surgeon who would be performing Avery’s surgery – 7 months! A few factors went into this, my daughter is on the smaller side, so she didn’t meet the requirements to have the surgery in our local hospital. The hospital that would perform the surgery was three hours away, with many other children on the waiting list for surgery. So all things considered 7 months wasn’t that long, but when you’re a parent having to force an NG tube into your child at least once a month, it seemed like a lifetime.
We met the surgeon in January 2022. The appointment was basically an opportunity for her to explain our options, the procedure and the risks to us. Offer information on the benefits and side effects of the g tube and for us to ask any questions we may have.
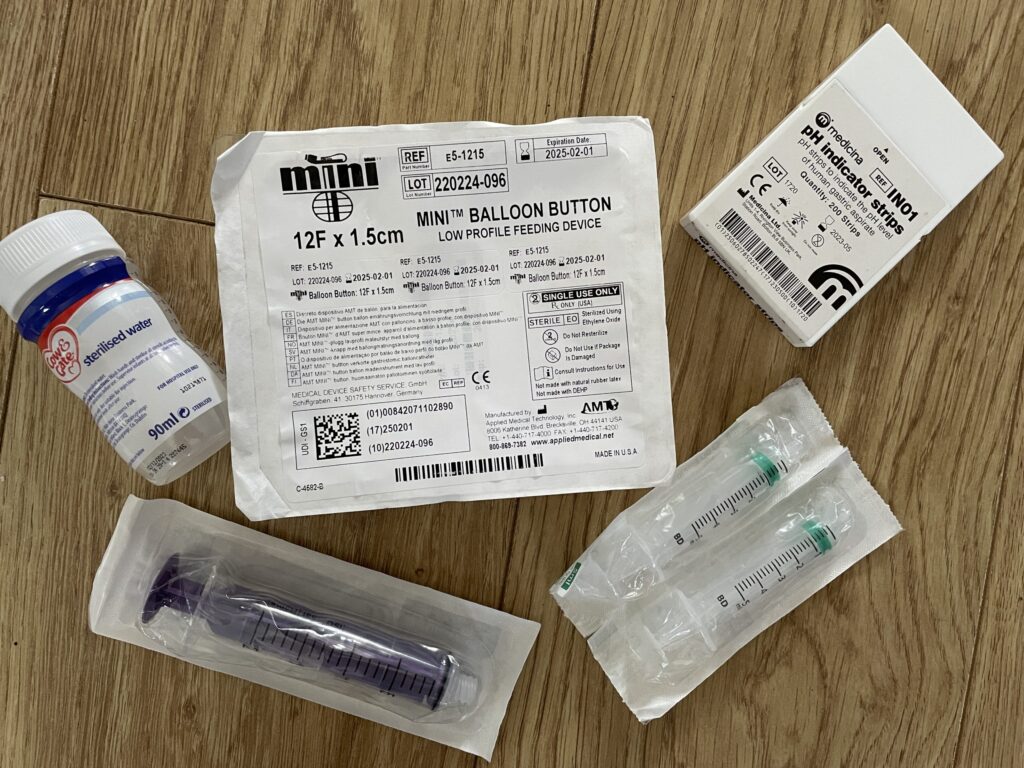
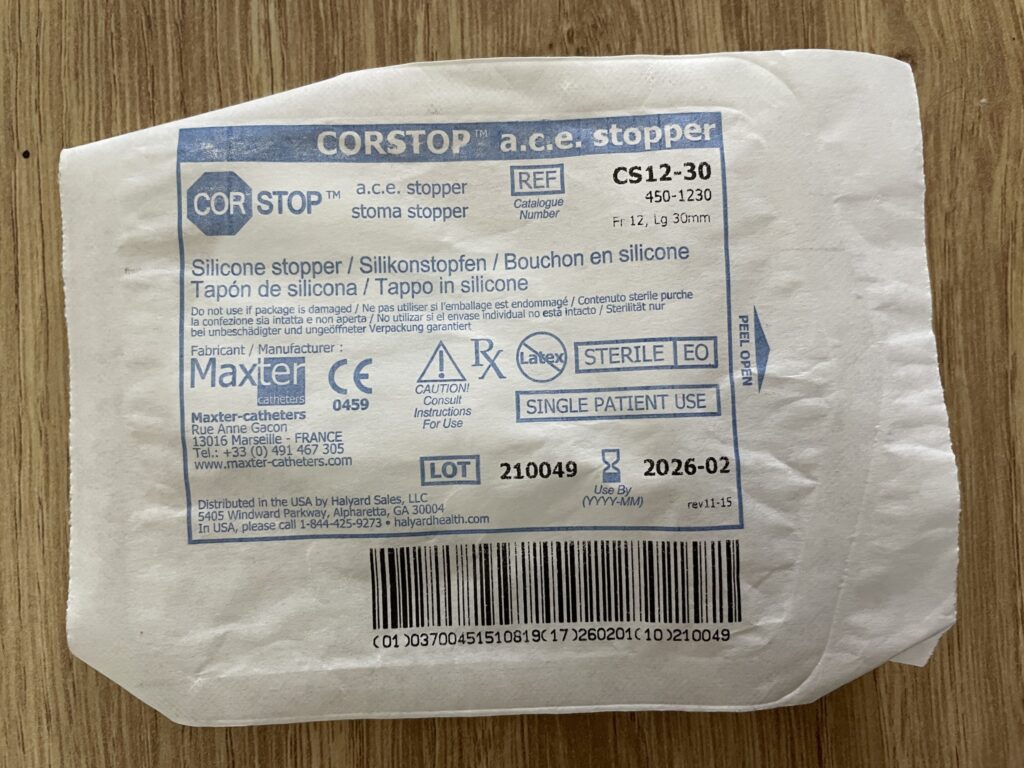
We agreed that Avery would have a primary button insertion, as opposed to a dangler style, Freka PEG g tube. It’s more common for a Freka to be inserted first, as it is a plastic disk that secures it, meaning no stitches are needed and it’s less likely to fall out. But this would mean Avery would need another surgery in 18 months for the Freka to be replaced with a button g tube.
The button was the end game for us, as it’s more low profile, and Avery has a very strong grip, we knew if she managed to get hold of a dangling tube, she could cause herself some damage.
The primary button insertion was a relatively new procedure for this hospital, after performing this method for around a year to a year and a half at the time of the appointment. But the surgeon assured me she was confident, and it would mean we would dodge the ordeal and discomfort of another surgery later down the line.
It did mean Avery would need stitches, and we would have to keep a very close eye on the button for the first couple of months, but it seemed like a good price to pay when weighing up our options.
Avery was placed on the waiting list, and due to her Reflux and aspiration risk she was a priority case. We were advised that we would expect a surgery date in the next three to four months, but we were warned we wouldn’t get much notice when the time came.
Prepping For Surgery
The surgeon was right, we didn’t get much notice. I think we received Avery’s surgery date with just under 2 weeks to spare. This didn’t give us a lot of time to arrange transport, accommodation for my husband and childcare for our older children.
We were advised not to feed Avery at all the day of her surgery, and considering we weren’t due to check into the ward until midday, we knew it was already going to be a long difficult day even before we got to hospital.
Surgery Day
We dropped our boys off with their Grandparents the night before and the day of the surgery we set off early for our three-hour drive to the Bristol Royal Hospital for Children.
When we arrived at hospital, Avery was checked into the day case ward. This is where my husband had to leave us, as because of the Covid restrictions, only one parent was allowed on this ward.
A nurse completed Avery’s observations and informed us that Avery was first on the list, so I assumed it wouldn’t be long until her surgery – I was wrong, and so was the nurse.
We waited and watched child after child be taken to theatre for their surgeries, turns out Avery was actually the last. I was incredibly irritated to say the least, Avery was tired and hungry, the youngest bar one in the ward, and I had clearly been misinformed. We waited in the day case ward for FOUR HOURS.
During that time the surgeon I met in January came to talk to me, she once again explained the risks, what to expect and I had to sign a few forms.

It was around 4pm when Avery was finally taken to theatre. We were taken to a small room and Avery sat on my lap while they used a mask to put her to sleep, I was grateful for this, as it meant she would already be asleep when they inserted a cannula.
There’s no feeling quite like your child being forced to sleep in your arms. This wasn’t my first experience, my son, Zachary has had a few general anaesthetics in his little life. Its’s not a nice feeling, its emotional and it feels kind of sad.
I laid Avery down, gave her a kiss and was shown out of the room. I was told I would get a phone call when the surgery was done, and I could come back to my daughter.
At this point I went to find my husband, who was aimlessly walking around Bristol city centre anxiously awaiting my call.
We tried to occupy some time and went to grab some food – on our way back to the hospital I received the call from the surgeon. Avery was out of surgery; it had gone as expected and she was happy with it. I was now able to go to Avery in the recovery room.
When I walked into the recovery room, I felt the guilt wash over me. My baby girl, still half asleep, was laying on a hospital bed that was way too big for her, she had an IV attached to a cannula in her hand, and her torso was covered in a big rectangular dressing. I noticed a tube sticking out of it that was connected to a drainage bag filled with brownish-red fluid.
The nurses assured me everything was normal, the IV was giving her fluids, to help rehydrate her after a full day of no food or water. The drainage was a normal colour, it was likely a bit of blood from the stoma site. The dressing would be kept on Avery’s stomach for two weeks, to give the stoma the best chance of healing.

Everything was normal, Avery was okay and the surgery went well. But I won’t lie – she looked weak, she looked tiny and she looked so very vulnerable.
Not long after this we wheeled Avery, still in the bed, to the general surgery ward, where she would spend the next few days.
Luckily this ward my husband was allowed on, and I was grateful for the support.
We moved Avery into the cot in her bed space, and shortly after she began to become more alert. It became obvious very quickly that Avery was in a lot of pain.
I had read in a Facebook support group that the staff won’t necessarily prescribe pain medicine other than the standard paracetamol and ibuprofen unless you ask for it – so you need to ask. I second this advice, we asked for Avery to be given stronger pain relief, explained that her body was already very much used to paracetamol, and they prescribed her with morphine.
After she was given the dose she immediately calmed down, relaxed and was able to go back to sleep. I’ll be honest, that first day I’m sure there was a point where both me and my husband wondered if we’d made the right decision.
But we had chosen this for a reason. These few days of pain will be forgotten, and Avery will benefit so much from having the g tube, I just struggled to see it that way at this moment in time.
Recovery
Those few days in the hospital kind of felt like they all rolled into one. They were hard – I struggled a lot, the nurses encouraged me to hold Avery as I normally would, but I was scared to hurt her. Avery is a baby that likes to be in your arms, but it was obvious she was in pain when I tried to cuddle her.
The nurses started to feed Avery through the g tube the day after her surgery, starting off low and slow and eventually building back up to her normal volume and rate before we were discharged home.
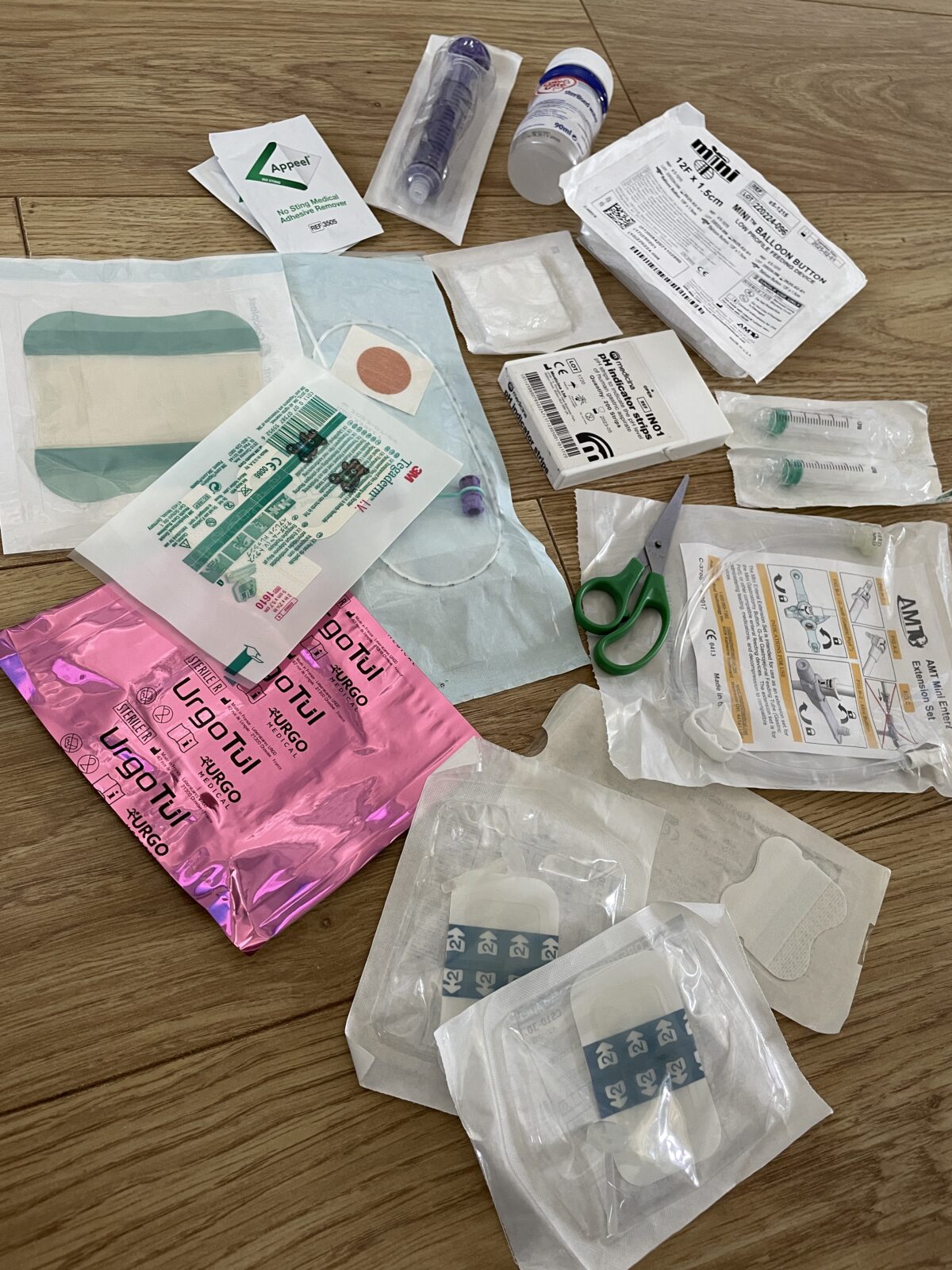
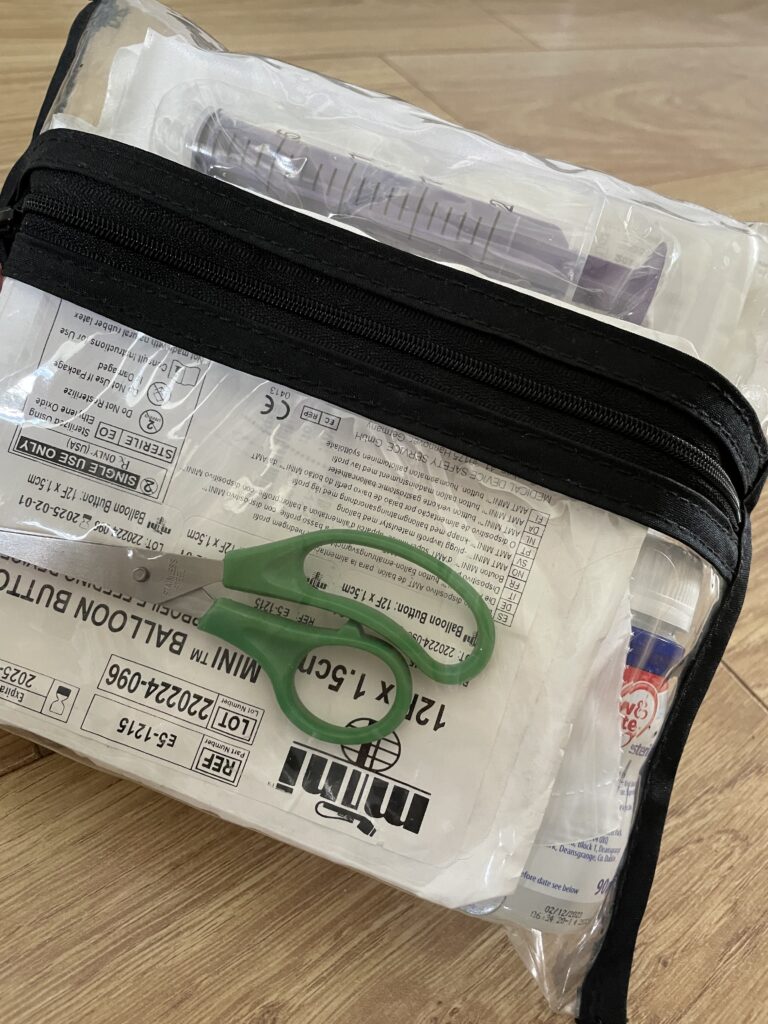
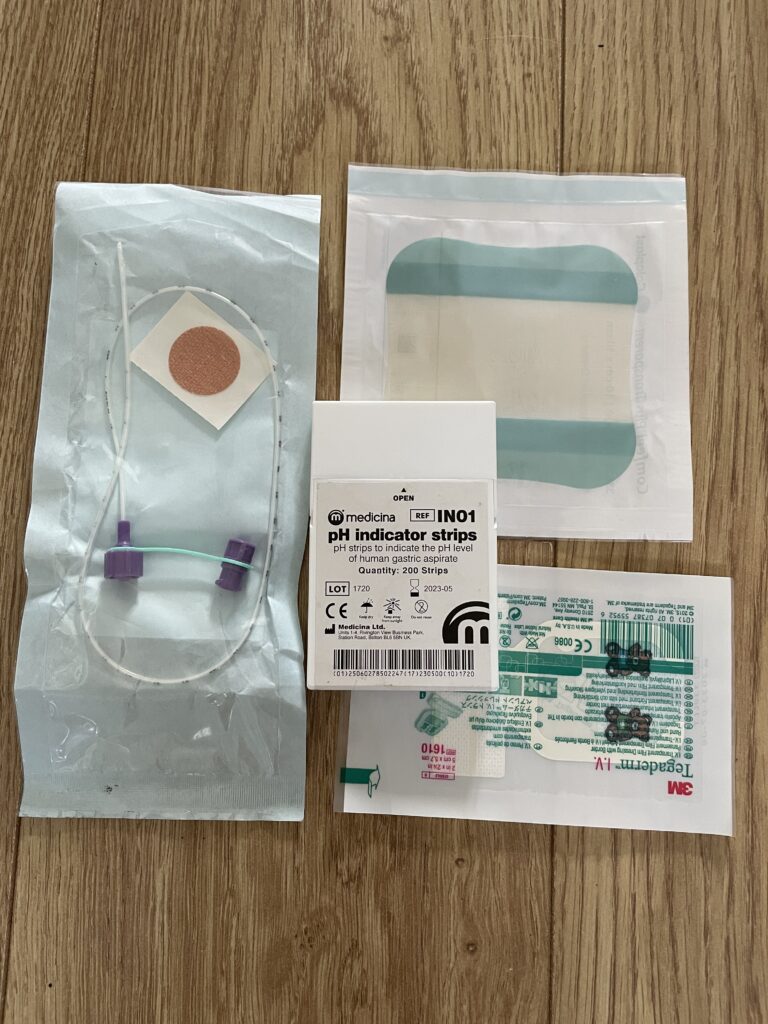
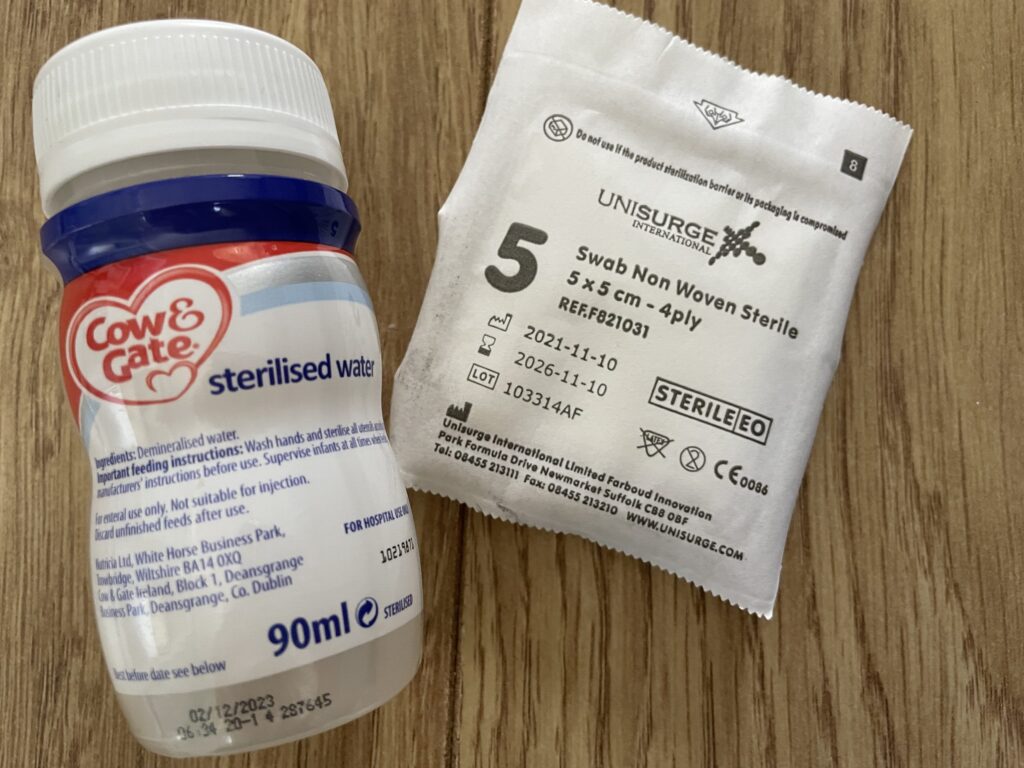
We saw a few different medical professionals, including Avery’s surgeon. We were trained on how to use the g tube, this was the easy part for us, as we were already so used to the NG tube, but still, we needed to complete an assessment before we could leave.
I was able to stay in the hospital overnight with Avery, I slept in a pull-out bed next to her. My husband on the other hand had to travel the three-hour round trip to Wales where he had family he could stay with.
The day we were discharged home I felt a little anxious. I knew how long of a journey we had to get home and Avery didn’t travel well at the best of times. It was obvious she was still uncomfortable, and once we left she would no longer have access to stronger pain relief.
The doctors and nurses all reassured me that Avery was ok, and that she’d be more comfortable at home at this stage.
They were right.
The journey home wasn’t as hard as I’d imagined, and once we were home, we settled Avery into her bouncer in front of her favourite movie – and she instantly seemed brighter.
Avery is now pretty much fully healed from her surgery. We had a few minor hiccups in the recovery process, including a prematurely ripped stitch and a few stoma infections. We’re also still trying to combat granulation tissue.
But I knew 100% that we had made the right decision the day we changed Avery’s button for the first time. She barely flinched, there was no pain, no tears, it was like she didn’t even feel it.
Th gastrostomy was the right decision for Avery and our family. You can tell my story that the surgery experience was hard, but that was to be expected. In my opinion is was worth it for the change we have seen in Avery ever since.